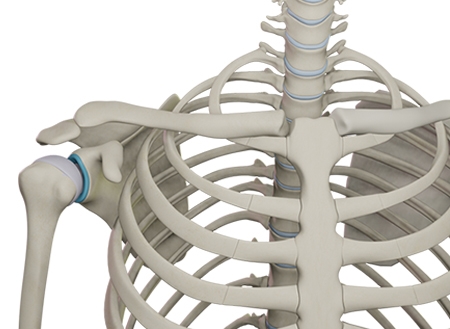
The shoulder is a complex joint that allows us great functionality due to its ball-and-socket anatomy. For those of us with relatively healthy shoulders, the multi-directional movement of the structures gives us the ability to scratch our back, reach a shelf above our head, buckle our seatbelt, and throw a ball. However, this mobility does come at a cost and that cost is instability. Instability can range from chronic hypermobility of the joint with daily activity to a subluxation (or partial dislocation of the joint) to a frank dislocation of the joint due to trauma that requires an external force to be reduced (or put back into place). Even something as seemingly mild as generalized hypermobility can make daily activities like putting on a jacket more difficult while also causing discomfort. Patients often report feeling unsettled when these instances occur. This general looseness of the shoulder joint is referred to as multidirectional shoulder instability, which is a chronic condition that does not result from one particular injury. This is a different type of instability from that caused by a traumatic dislocation of the shoulder.
This generalized instability without injury is caused by the humeral head (the ball of the joint) not staying centered in the glenoid (or socket of the joint). Those most likely to struggle with this multidirectional instability of the shoulder are adolescent females. People who have genetic disorders like Ehler-Danos or Marfan Syndrome are also more likely to experience hypermobile joints. The diagnosis is clinical, meaning that advanced imaging studies are not necessary to confirm the diagnosis. Rather, your physician will determine the diagnosis after hearing a patient’s reported symptoms and performing a physical examination of the joint. In some cases, an MRI may be ordered if the instability is great enough that concern for structural damage exists. Otherwise, x-rays are typically sufficient.
The good news about this instability is that it rarely requires surgical intervention. Most often, an extensive bout of physical therapy to improve the general mechanics of the shoulder will improve or even resolve symptoms. Physical therapy will work on dynamic stabilization as well as scapular mechanics to help the soft tissue structures surrounding the shoulder joint better hold the joint in place. As the musculoskeletal system matures, the instability usually corrects itself. It is only in few and far between cases that a patient continues to struggle with significant and limiting symptoms that are not improved by physical therapy. For those patients, surgical intervention in the form of a capsular shift or capsular plication could be considered. These two procedures are simply different methods of tightening the capsule of the joint to allow less motion of the shoulder. These procedures require general anesthesia and a recovery period to follow. The trade-off of improved stability of the joint is decreased motion, so patients who are throwing athletes typically do not pursue such measures. Surgery is not typically performed until extensive physical therapy has been completed.
If you have a shoulder that ‘pops’ in and out, come see one of our shoulder specialists. They can confirm the degree of instability and get you set up with a physical therapist to help you stabilize the joint and get back to uninterrupted activity.
This blog is written by one of our very own-Morgan. She is a certified athletic trainer working in our clinic with our providers each and every day. She obtained a bachelor’s degree in athletic training from Carroll University in Waukesha and a master’s degree in Kinesiology from Michigan State University.