Today’s blog is going to enter into the realm of physiatry. We have two physiatrists at our practice: Dr. Zoeller and Dr. Vo. They are specialists in physical medicine and rehabilitation.These two gentlemen have plenty of tricks up their sleeves for helping patients find therapies and treatments that alleviate symptoms from pathologies that cannot necessarily be helped by surgical intervention.
One of the treatments our physiatrists offer is radio frequency ablation (RFA). This is an outpatient procedure used to treat chronic pain in the spine or a painful joint, usually the knee. Sometimes patients have an arthritic joint that can not be replaced due to comorbidities or other circumstances. If other conservative measures have been exhausted and surgery is out of the question, the patient may be referred for an RFA.Other patients have already undergone a knee replacement, but for whatever reason, the surgery was not successful in improving the discomfort. If revision of the replacement is not an option, perhaps RFA is. Patients with chronic back pain can also be candidates for this procedure.
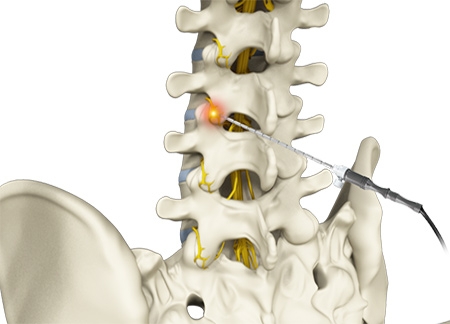
RFA uses high frequency pulsed radio waves to burn the nerves that carry pain signals to the brain. Without these nerves intact and able to transmit signals, the pain should not be felt. This technique still allows the body to move normally because the nerves that innervate (or control)the area are still intact. The procedure allows function without discomfort.
Prior to proceeding with this procedure, the physician will first perform a nerve block in the associated area to confirm that the presumed area is indeed causing the pain. Sometimes referred pain from other areas is a contributing factor.If referred pain exists, the RFA may notalleviate the discomfort because of complicating factors and perhaps multiple sources of pain. Ifa patient reports that the nerve block alleviated his or her symptoms, then the physiatrist will likely proceed with the procedure, confident that it will improve symptoms.
This procedure is done in an outpatient setting and is minimally invasive. The patient will lie on an x-ray table in a sterile procedural room as this procedure is done using fluoroscopy guidance to ensure appropriate needle placement. The current is transmitted through the inserted need to burn (or otherwise destroy) the associated nerve,which renders the nerve unable to transmit.The procedure itself only takes a couple minutes to perform. The relief is usually temporary as these nerves can eventually recover and start transmitting pain signals to the brain once again.Ideally, patients receive at least six months of relief.Lots of patients receive a year or more of relief.
The procedure is a little more painful than a standard cortisone injection that might be administered in a clinic exam room. The soreness and tightness usually only lasts about a week. It is at that point that patients start noticing some pain control. No limit exists to how many RFA procedures can be performed on a single body part.The decision to proceed with this treatment is made by the physician and patient after weighing risks and benefits. It is our goal to provide our patients with a plan that helps them continue to live an active and independent lifestyle by providing appropriate treatments to alleviate symptoms and restore function. If you think RFA may be appropriate for you, give us a call to schedule with one of our physiatrists today!
This blog is written by one of our very own-Morgan.She is a certified athletic trainer working in our clinic with our providers each and every day. She obtained a bachelor's degree in athletic training from Carroll University in Waukesha and amaster's degree in Kinesiology from Michigan State University.